Dying People and a Dying Health System: The Impact of Protracted State Violence on Health in Gaza

by A Woods
Israeli state violence and the apartheid blockade have been fuelling a humanitarian crisis in Gaza for many years, with perpetual cycles of destruction and human suffering. Rather than focussing on the intricacies of Israeli state criminality (see State Crime Journal Volume 5, Issue 1), this piece aims to shine a light on how the health of the two million people living in the Gaza Strip has been affected. The detrimental impact of the conflict on health goes much further than the deaths, injuries and disability seen during surges in violence; it ravages whole health systems, infects the environment, and causes multiple generations of trauma.
This piece will begin by exploring the impact of protracted Israeli state violence (including the blockade) on the Gazan healthcare system itself. The effects are multi-layered. Chronic neglect, exacerbated by the blockade, has left the health system stunted and underdeveloped, and each new surge in violence causes further degradation. The routine bombing of civilian targets (including hospitals and UN facilities) adds further strain to services, damages health infrastructure and endangers the lives of healthcare workers. The piece then moves on to evaluate how this violence impacts the health of Gazans through displacement and shortfalls in water, sanitation and hygiene (WASH) services. Once more, when assessing the living conditions in Gaza a pattern of chronic issues exacerbated by acute conflict emerges. Crises layered upon years of neglect. The piece concludes by evaluating how these mechanisms combine to detrimentally affect the health of Gazans from multiple angles.
Gazan Healthcare System: ‘The Only Stable Thing is Instability’ (Dr Kashif, international liaison with the Gazan MoH)
To understand the health impacts on individuals, we must zoom out and look at the effects of protracted state violence on the Gazan healthcare system. Each Israeli military escalation brings it closer and closer to the brink of collapse, but what are the root causes of the health system’s longstanding instability?
Chronic Neglect of the Healthcare system
Understanding the long-term neglect of the healthcare system means appreciating that its history is intertwined with the area’s socio-economic and political history. Gaza has been ruled by several different regimes, each with an influence on healthcare provision (see text box for a brief overview of how the system has changed over the last century).
|
Gazan Healthcare System over Time British Mandate Period, 1920–48 The Government Department of Health under the British Civil Administration provided health services. Gaza under Egyptian administration, 1948-67 With the West Bank under Jordanian control and Egypt occupying the Gaza Strip, two separate health systems started to develop. The events of 1948, known as Al Nakba (‘The Catastrophe’) to Palestinians, led to the creation of around 750,000 Palestinian refugees. In 1950, the United Nations Relief and Works Agency for Palestine Refugees (UNRWA) was established to provide health services to these refugees. Israeli Administration, 1967-94 Following Israeli occupation, the military authorities took over the governmental healthcare system, administering it in way that kept it stunted and underdeveloped. The governmental allocation for health services was far below that of Israel and was the second lowest of 36 low-income and lower-middle-income countries at the time. In 1986, the average expenditure on health services in the West Bank and Gaza Strip was below US$30 per person per year, compared to US$350 per capita in Israel (Giacaman, 1994). The UNRWA was able to develop its own system of basic services for the refugee population. Health system under the Palestinian Authority, 1994 Beginning in 1993, the Oslo Accords were an attempt to mediate the conflict, leading to the creation of the Palestinian National Authority (PNA). Certain powers such as healthcare provision were transferred from Israel to the PNA. In 1994, the Palestinian Ministry of Health (MoH) was established, inheriting the neglected health services from the Israeli military government. After 1994, Israel claimed to have no obligation to the well-being of Gazans, despite the Geneva Conventions stating that Israel as the occupying power was responsible for the health of the population. This vacuum of responsibility resulted in a fragmented patchwork of healthcare providers: the MoH, non-governmental organisations (NGOs), UNRWA and the private sector. The situation was further complicated by the Islamic Resistance Movement (Hamas) takeover of the Gaza Strip in 2007, splitting the PNA into two governing structures: Fatah in the West Bank (internationally recognised and supported), and the Hamas government in the Gaza Strip. As a result, Israel introduced a severe blockade and military measures on Gaza, and the international community implemented a political and financial boycott. |
De-development and the Blockade
The Israeli occupation of the Gaza Strip has lasted over half a century. This has not just distorted development in Gaza, but has prevented and reversed any independent development through the deliberate deconstruction of Gaza’s economy – termed ‘de-development’ by Sara Roy (Roy, 2016). Beginning in 1967, this process has since been intensified by the 15-year land, air and sea blockade that has trapped over two million people inside Gaza since 2007. The previous UN Chief Ban Ki-Moon has referred to this open-air prison as ‘collective punishment’ – a breach of humanitarian international law (the Geneva Conventions). Moreover, a recent report by the Special Rapporteur on human rights in the Palestinian territories has concluded that the political system of entrenched rule in Gaza amounts to apartheid, calling for its immediate dismantlement (UN Human Rights Council, 2022).
The Israeli siege on Gaza has created extreme economic dependency. Many Palestinians relied on work outside of the Gaza Strip, resulting in a 45% unemployment rate, 60% poverty rate, and the majority of the population dependent on international aid (The World Bank, 2021). The blockade also prevents Gaza from trading with the outside world, whilst forcing the population to be a captive market for Israeli goods. This creates a situation where Gazans may solely act as consumers – an unsustainable situation given that without the opportunity to earn income, the population will not have the capital to purchase goods. This undermines Gazan sovereignty, contributing to the process of de-development. Similarly for healthcare provision, a complete reliance on Israel and outside donors has been created for medical items, with constant uncertainty of availability of supplies (Smith, 2015).
In addition to these immediate shortages of supplies, the health system itself has also been severely weakened. A joint health cluster assessment concluded that the blockade has severely inhibited health sector development, and the rebuilding of the health service will be impossible whilst the blockade is in place (WHO, 2014). The report highlights the lack of training opportunities for medical staff and the deterioration of health infrastructure.
International aid, donor focus and neoliberal processes also play a role in the process of de-development. Critics argue that neoliberalism can shift control from local authorities to the private sector, leaving ‘governance voids’ (Cliffe and Luckham, 2000), as seen with the limited capacity of the Hamas government to provide health services. This gives rise to ‘disaster capitalism’, where the value of the private sector increases as the public sector becomes increasingly destabilised (Klein, 2007). In Gaza, this is illustrated by the increasing number of civil society actors, who can be influenced by both local political agendas and wider geopolitics. This is not to say that humanitarian interventions are not vital in fragile conflict settings like Gaza, as they provide much needed support and alleviate the short-term effects of socioeconomic crisis. However, the way aid is provided and its associated politics may hinder the long-term development of the public sector. Donor-driven agendas mean projects tend to serve funders rather than recipients. For example, funding is more likely to go towards projects with short timelines and rapid results, rather than towards sustainable programmes which improve the healthcare system itself (Hammoudeh et al., 2020), as observed in Gaza. Although this policy may save lives in the short-term, it simultaneously prevents the Hamas government from achieving any long-term social or economic progress, intensifying economic dependence (Qarmout and Béland, 2012; More, 2006). This links to the concept of aid conditionality, where donors can stipulate political or economic changes from the recipient (Selbervik et al., 1999). Therefore, donors have isolated and weakened the Hamas-led government by strictly allocating funds to emergency relief and forcing agencies to limit contact with Hamas representatives (Qarmout and Béland, 2012). UN agencies were also obliged to follow this policy due to the international community’s boycott[1] (Giacaman et al., 2009). The resultant inadequacies of the public sector then feed back into the justification of privatisation under neoliberalism, creating a vicious cycle that continues the de-development of the Gazan healthcare system.
At worst, conditional aid in Gaza has compromised the presumed politically neutral role of aid agencies by being used to undermine the Hamas government. At best, aid agencies have failed to successfully challenge the blockade and have allowed Israel to continue its occupation and bombing campaigns without having to provide for the health needs of Gazans. As Mark Levine put it, the lack of responsibility shown by Israel for the health of Gazans means Israel continues to ‘eat its territorial cake and still have it’ (LeVine, 2016).
In summary, Israeli occupation, violence, the blockade and unsustainable aid have contributed to decades of de-development in Gaza, hampering healthcare provision through two interlinked processes: superficially, the restricted movement of people and resources, and most significantly, the undermining of healthcare at a systems level through marginalisation of the Ministry of Health (MoH).
Implications for the Gazan Healthcare system
What does all this mean for the Gazan healthcare system and the two million people that rely on it in the face of conflict and violence? How can the effect of decades of neglect combined with recent destruction be evaluated? The World Health Organisation (WHO) has a framework which splits a health system into its building blocks – ‘service delivery’, ‘health workforce’, ‘information’, ‘medical products, vaccines, technologies’, ‘financing’ and ‘governance’ (World Health Organization, 2007) – thus helping to visualise the multiple dimensions of a health system. In this piece, this framework has been adapted (Figure 1) in order to evaluate how conflict in Gaza has impacted the health system on every one of these levels. Inadequacies in one building block then has repercussions on other levels, multiplying their impact. Remove blocks and a structure crumbles. The Gazan health system is crumbling, and it is only a matter of time before it collapses fully.
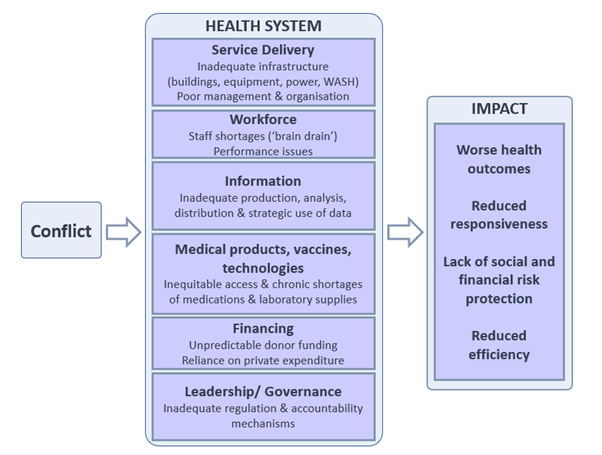
Figure 1: Adapted version of WHO building blocks framework to illustrate the impact of conflict on the Gazan health system and the resultant health impacts.
Using this framework, a pattern of chronic issues exacerbated by acute bouts of conflict emerges.
- Service delivery
Good health services are those which deliver effective, safe, quality health interventions in an equitable manner. In Gaza, this is hampered by inadequate infrastructure and poor management and organisation.
Health infrastructure – ranging from buildings, equipment and power supply to water, sanitation and hygiene (WASH) services – has been neglected for many years and suffers further damage with each escalation in hostilities.
Targeting healthcare facilities has become a deliberate military strategy worldwide. In Gaza, damage to facilities from routine Israeli bombing campaigns has reduced service availability, adding extra pressure to the remaining functioning facilities. For example, the surge in violence from Operation Protective Edge in 2014 left the al-Wafa Rehabilitation Hospital (Figure 2) completely destroyed from the air (Dyer, 2014). A joint health cluster assessment concluded that 73 hospitals and primary health clinics were damaged and 45 ambulances were destroyed. The estimated cost of destroyed health infrastructure, excluding medical equipment and material, was US$12,063,250 (WHO, 2014). At the height of the conflict, 45.7% of all public health facilities were unable to provide services (ibid). In the context of Gaza’s weakened economy and healthcare system, these costs and service delivery reductions are even more significant.

Destroyed Al Wafa Rehabilitation hospital, 2014, MAP
An editorial by the Lancet highlights the similar effects of Operation Cast Lead, when an estimated 34 health facilities were damaged or destroyed during the 22-day conflict (Mason, 2009; The Lancet, 2009).
Compounding this, the blockade reduces the capacity to rebuild infrastructure by restricting building materials such as cement (Dyer, 2014). Medical equipment damaged during conflict also exacerbates the chronic maintenance issue in Gaza resulting from restrictions on importing spare parts (WHO, 2014).
Moreover, the health sector suffers from frequent power cuts, compounded by fuel shortages for backup generators due to the blockade. As a result, many hospitals were forced to shut down areas such as operating theatres, emergency departments and wards (UN Human Rights Council, 2018). In August 2020, Israeli authorities stopped the entry of most goods into Gaza, including fuel, leading to the shutdown of the Gaza Power Plant and consequent power cuts for up to 20 hours a day (UN OCHA, 2020).
Water, sanitation and hygiene (WASH) facilities in healthcare settings are also of significant concern. An assessment study by UNICEF of healthcare facilities in Gaza found numerous cases of water contamination and lack of access to basic sanitation services (UNICEF & WW-GVC, 2019). Another study found worrying evidence that suggests bacteria resistant to many antibiotics are being transmitted through these inadequate WASH services (Shomar, 2021).
Health service also relies on management and organisation of provider networks. The aim of management is to maximise service coverage, quality and safety, whilst minimising waste. This goes hand in hand with an organised provider network to ensure continuity of care and avoid unnecessary duplication of services. As discussed, Israeli state violence and the blockade in Gaza have resulted in inconsistent management of the healthcare system, with a historic failure to promote Palestinian leadership capacity (see previous sections ‘Chronic Neglect of the Healthcare System’ and ‘De-development and the Blockade’). The lack of a sustainable development agenda has compromised strategic planning, resulting in a fragmented health sector with multiple partners, including the UNWRA, NGOs, the private sector and the marginalised MoH. Organisation is also impeded by conflicting donor agendas and poor coordination between agencies.
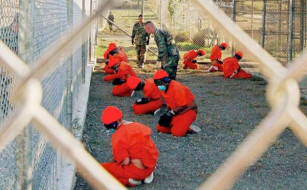
Service delivery shortages in Gaza are compounded by complicated referral systems. Permits must be requested for patients to receive healthcare outside of Gaza; increasingly, these requests are delayed or rejected by Israeli authorities (WHO, 2018). The Great March of Return 2018-19 resulted in over 36,000 injuries, with over 7,000 limb gunshot wounds requiring complex treatments. This far exceeded the capacity of the Gazan healthcare system, meaning many patients’ lives depended on approval to leave Gaza for specialised treatments. Many patients were not granted exit permits – of the 604 applications, 28% were rejected and 55% did not receive an answer in time for the appointment (UN OCHA, 2020).
- Health workforce
There are critical shortages of healthcare professionals in Gaza. Staff working in Ministry of Health (MoH) facilities are often lost to NGOs and the private sector, resulting in a ‘brain drain’ (Smith, 2015; Mataria et al., 2008). This is partly due to salary cuts and irregular wages. Since 2014, Gaza-based MoH staff have been receiving only 40% of their total monthly salary every 40 to 50 days (UN OCHA, 2018). This is as a result of the financial crisis of the MoH and the preference of donors to pay for tangible goods rather than salaries (Smith, 2015).
There is also a drain of medical staff leaving Gaza itself, due to poor living conditions and deteriorating health system. In 2018 alone, 84 doctors left Gaza (WHO, 2019). This chronic human resource problem is exacerbated by access issues during surges in Israeli violence, when staff transport to work is disrupted because of security issues and lack of fuel. Health worker safety is also at constant risk. During Operation Protective Edge, grave breaches of International Humanitarian Law led to the deaths of 23 health workers, with a further 83 injured (WHO, 2014). During the Great March of Return, 845 health workers were injured (Shehada et al., 2021) (Figure 3).

Health workers attacked during the Great March of Return demonstrations, 2019, MAP
Inevitably, these shortages impact the performance of staff. Staff shortages reduce the quality of services provided and increase the workload of remaining staff. Surges in Israeli state violence further increase exhaustion levels, and redeployed staff may lack the knowledge and experience to work in their new environments (WHO, 2014). The blockade reduces opportunities for staff to receive external training, potentially reducing performance (Smith, 2015; Summerfield et al., 2018) – yet another form of de-development.
- Information systems
A well-functioning health information system facilitates the production, analysis, distribution and strategic use of health data. Electricity shortages, infrastructural damage, the destruction of patient records and administration staff shortages as a result of conflict in Gaza impede the collection of data and its application in health policy (WHO, 2014). The implications of this are huge; without a health information system there can be no early warning system for disease outbreaks, there is no data to guide planning of services or to monitor quality standards, there can be no research to inform education and training, improve health outcomes or uncover trends and health inequities. Reliable information is the foundation for decision-making across all health system building blocks, yet data generation and application in Gaza is severely hampered by the conflict.
- Medical products, vaccines, technologies
Equitable access to quality, safe and effective medical products, vaccines and technologies is an important aspect of a healthcare system. Chronic shortages are exacerbated by increased demand during surges of violence (WHO, 2019; UN Human Rights Council, 2018). Israel’s blockade and the subsequent financial crisis of the MoH has eradicated the ability of Gaza to manufacture its own pharmaceuticals; this increases dependency on the occupying power Israel and outside donors (Smith, 2015). Compounding this, the Palestinian MoH has to pay higher prices for medicines compared to international benchmarks, due to import restrictions (UN Human Rights Council, 2018). Israel also restricts the entry of items that may have military usage – including building materials such as cement and certain medical equipment – resulting in an unpredictable supply chain and long delays following a lengthy application and review process. In 2019, 42% of essential medicines categories were completely depleted and 26% of essential medical disposables were below a month’s supply (WHO, 2020).
Perhaps one of the most ominous concerns is the shortage of antibiotics. Gazans are left with no choice but to use counterfeit or low-quality products, which is not only ineffective for curing their illness but also contributes the emergence of antibiotic resistance. These resistant strains may be able to spread to other countries, as observed in the past with previous wars in the Middle East (Zorgani, 2013; Peretz et al., 2014; Sahli et al., 2016; Ecker et al., 2006; Turton et al., 2006; Gostev et al., 2021). Poor healthcare provision in one part of the world can drive antibiotic resistance globally; until the burden of infectious diseases in places like Gaza is reduced, a global pandemic of antibiotic resistance remains a threat to us all.
- Financing
A sustainable health financing system ensures people can use services whilst being protected from severe financial hardship (meaning the system aims to remove financial barriers to disadvantaged populations and ensures the cost of medical treatment does not send patients and their families into poverty). The financial accessibility of health services is compromised in Gaza, and inequities will undoubtedly continue to increase as poverty and unemployment rise. Protracted conflict in Gaza has led to fragmentation the health financing system, making risk pooling a challenge and resulting in unequal burdens (Abu Zaineh, 2009). Public spending on health relies heavily on unpredictable donor funding (Smith, 2015), which increases reliance on private expenditure (World Bank, 2016). Increasing numbers of patients in Gaza are having to pay for their healthcare with no financial support; since 2000, out-of-pocket payments (where the patient must pay for health services at the point of access from their own savings) have consistently contributed to approximately 40% of health expenditure in Palestine each year (Palestine Central Bureau of Statistics, 2022).
- Leadership/ governance
The leadership and governance of health systems is one of the most complex but critical building blocks, overseeing policy, regulation, system design and accountability. It has already been discussed how the de-development of the Gazan health system has resulted in poor governance (see previous section ‘Development and the Blockade’), causing inconsistent management and inadequate organisation of services and human resources. Another shortfall in this area lies in policy and regulation.
A policy vacuum in Gaza has enabled the growing influence of the World Bank in its economic and social sectors, including health (Giacaman et al., 2003). The World Bank’s policy, directed towards a free-market economy, has increased the importance of the private sector. Regulation and policy implementation is impeded by unstable leadership, limited resources and the prioritisation of emergency needs over sustainable governance during acute bouts of violence (Truppa and Abo-Shehada, 2020; Giacaman et al., 2003). The fragmentation of health providers also risks diffusing responsibility.
Environment: ‘Gaza Unliveable by 2020’
Health is not only impacted by shortfalls in the healthcare system, but also by the abysmal living conditions of the Gaza Strip. In 2012, the UN estimated that Gaza would be unliveable by 2020 (United Nations Country Team in the occupied Palestinian territory, 2012). Since then, a follow-up report found that living conditions were deteriorating even faster than anticipated, accelerated by numerous rounds of hostilities (UN Country Team in the occupied Palestinian territory, 2017). It is now 2023 and it is evident that the humanitarian situation in the Gaza Strip is even more dire, yet over two million people, including almost one million children, are still ‘living’ in this ‘unliveable’ place.

Destroyed apartments in Gaza City, 2021, MSF
Displacement
It is well-known that conflict displaces large numbers of people, either internally or as refugees, threatening their safety, wellbeing and human rights and hindering their socioeconomic development. Displacement increases the exposure of populations to new infections and environmental contamination (Garry and Checchi, 2019; Gates et al., 2012). Overcrowding of temporary accommodation increases disease transmission, whilst malnutrition and stress caused by insecurity compromise people’s immune systems (Ghobarah et al., 2003).
Protracted conflict in Gaza has created large-scale displacement. Of a population of 2.1 million people, 1.4 million are refugees (United Nations Relief and Works Agency for Palestine Refugees in the near East, 2022). Acute surges in state violence cause further displacement. Following Operation Protective Edge in 2014, over 350,000 people were displaced into overcrowded shelters (WHO, 2014), on top of over 2,000 Palestinian deaths. Compounding this, movement out of Gaza is significantly more limited due to its closed borders; combined with the small size of the territory, this creates a high population density, undermining infection control efforts and placing further stress on the crumbling healthcare system.
Water, Sanitation and Hygiene (WASH)
The impacts of displacement are compounded by the disruption of protective factors due to conflict, such as access to WASH services.
Since 1967, Palestinian water development has been under Israeli military control (UN Human Rights Council, 2019), resulting in a deterioration that mirrors that of the health system. There are three main sources of fresh water in the Occupied Palestinian Territory: the Jordan River, the mountain aquifer and the coastal aquifer. Israel prohibits Palestinian access to water from the Jordan River, and the mountain aquifer is located primarily in the West Bank. The coastal aquifer, the only remaining source of natural drinking water for Gazans, has been severely compromised by contamination with sewage and seawater (Human Rights Council, 2022; UN Country Team in the occupied Palestinian territory, 2017). This is due to Israeli imposed power shortages impeding the waste treatment system, allowing untreated wastewater to be discharged into the Mediterranean Sea (UN OCHA, 2021). In 2021, over 97% of the water from the coastal aquifer did not meet WHO water quality standards. This increases the risk of waterborne disease and leaves only 4.3% of Gazans with access to safely managed water (Palestinian Central Bureau of Statistics (PCBS) and Palestinian Water Authority (PWA), 2021). A RAND Corporation report found that more than 25% of reported diseases in Gaza are the result of reduced availability and quality of water (Efron et al., 2019). Access is projected to decrease further with climate change, with disproportionate effects on poorer groups who cannot afford the cost of trucked water (UN Human Rights Council, 2020).

Water crisis in Gaza, 2016, Palestinian Water Authority
As observed in healthcare facilities (see previous section ‘Implications for the Gazan Healthcare System: Service Delivery’), there is also insufficient access to sanitation and hygiene services at the household level (UN OCHA, 2021; UN General Assembly, 2021). Infrastructure has been chronically neglected, and then further damaged during military campaigns. The blockade poses similar problems for repairs as it does in the health sector, by restricting the import of spare parts (Efron et al., 2019). These poor living conditions deteriorate further when mass displacement causes overburdening of WASH facilities in IDP shelters.
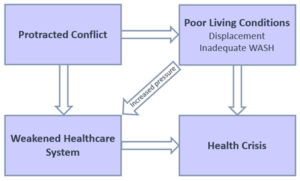
Figure 2: Summary – The contribution of conflict to the health crisis in Gaza, via the health system and living conditions
A Summary and Plea
In Gaza, de-development, the blockade and destruction by persistent Israeli military incursions are continuously contributing to the deterioration of living conditions. The combined effects of displacement and inadequate WASH services act synergistically to negatively impact the health of Gazans. The weakened health system is not equipped to cope with this increasing strain, especially when faced with large numbers of casualties during escalations in violence.
Explosive weapons and live ammunition have caused thousands of deaths in Gaza over the years, yet the catastrophic long-term health impacts of the conflict leave craters in the health system itself, hampering the ability of generations of Gazans to heal. A long history of socioeconomic and political instability plus the added implications of the blockade has left the health system stunted and underdeveloped, unprepared for the constant fluctuations in conflict which repeatedly bring it to the brink of collapse. Analysis using the WHO building blocks framework illustrates how every dimension of the system has been affected, from infrastructure and workforce to whole information systems and governance.
For both the health system and living conditions, there is a clear pattern of chronic neglect exacerbated by acute bouts of conflict, ultimately leading to the deterioration in health of the Gazan population.
For decades, Israel’s state crimes have been cloaked in denial (Cohen, 1993); however, the devastating effects of these crimes on the health of Gazans is profoundly clear, and their right to health cannot be denied.
The Israeli state’s apartheid project is directly responsible for the medical crisis faced by those living in Gaza and until the international community confronts Israel’s crimes the misery for Gaza’s estimated 2 million inhabitants will continue. At the same time, the immediate importance of providing sustainable aid in the right places, in the right way, cannot be understated. The international community must also support Gaza to improve healthcare at a systems level, increasing long-term resilience as well as providing short-term emergency aid. In addition, efforts must be concentrated outside of the health sector, improving the living conditions in Gaza through sustainable investment in water, sanitation and hygiene services. The multiple mechanisms by which health is affected means there are multiple opportunities for improvement – we must take these opportunities before it is too late, and the Gaza Strip becomes truly ‘unliveable’.
REFERENCES
Abu Zaineh, M. 2009. Contribution to the analysis of health equity: measurement and explanation of inequality and inequity in the health care sector in the context of developing countries: the Palestinian case. Birzeit University. Center for Development Studies.
Cliffe, L. & Luckham, R. 2000. What happens to the state in conflict?: Political analysis as a tool for planning humanitarian assistance. Disasters, 24, 291-313.
Cohen, S. 1993. Human Rights and Crimes of The State: The Culture of Denial. Australian & New Zealand Journal of Criminology, 26, 97-115.
Dyer, O. 2014. Rebuilding health services in Gaza won’t be possible while Israel maintains blockade, says report. BMJ : British Medical Journal, 349, g6644.
Ecker, J. A., Massire, C., Hall, T. A., Ranken, R., Pennella, T. T., Agasino Ivy, C., Blyn, L. B., Hofstadler, S. A., Endy, T. P., Scott, P. T., Lindler, L., Hamilton, T., Gaddy, C., Snow, K., Pe, M., Fishbain, J., Craft, D., Deye, G., Riddell, S., Milstrey, E., Petruccelli, B., Brisse, S., Harpin, V., Schink, A., Ecker, D. J., Sampath, R. & Eshoo, M. W. 2006. Identification of Acinetobacter species and genotyping of Acinetobacter baumannii by multilocus PCR and mass spectrometry. J Clin Microbiol, 44, 2921-32.
Efron, S., Fischbach, J. R., Blum, I., Karimov, R. I. & Moore, M. 2019. The Public Health Impacts of Gaza’s Water Crisis: Analysis and Policy Options. Rand health quarterly, 8, 10-10.
Garry, S. & Checchi, F. 2019. Armed conflict and public health: into the 21st century. Journal of Public Health, 42, e287-e298.
Gates, S., Hegre, H., Nygård, H. M. & Strand, H. 2012. Development Consequences of Armed Conflict. World Development, 40, 1713-1722.
Ghobarah, H. A., Huth, P. & Russett, B. 2003. Civil Wars Kill and Maim People—Long After the Shooting Stops. American Political Science Review, 97, 189-202.
Giacaman, R. 1994. Health conditions and services in the West Bank and Gaza Strip: study/prepared by Rita Giacaman, UNCTAD consultant.
Giacaman, R., Abdul-Rahim, H. F. & Wick, L. 2003. Health sector reform in the Occupied Palestinian Territories (OPT): targeting the forest or the trees? Health Policy and Planning, 18, 59-67.
Giacaman, R., Khatib, R., Shabaneh, L., Ramlawi, A., Sabri, B., Sabatinelli, G., Khawaja, M. & Laurance, T. 2009. Health status and health services in the occupied Palestinian territory. The Lancet, 373, 837-849.
Gostev, V., Ivanova, K., Kruglov, A., Kalinogorskaya, O., Ryabchenko, I., Zyryanov, S., Kalisnikova, E., Likholetova, D., Lobzin, Y. & Sidorenko, S. 2021. Comparative genome analysis of global and Russian strains of community-acquired methicillin-resistant Staphylococcus aureus ST22, a ‘Gaza clone’. International Journal of Antimicrobial Agents, 57, 106264.
Hammoudeh, W., Kienzler, H., Meagher, K. & Giacaman, R. 2020. Social and political determinants of health in the occupied Palestine territory (oPt) during the COVID-19 pandemic: who is responsible? BMJ Global Health, 5, e003683.
Human Rights Council 2022. Report of the Special Rapporteur on the situation of Human Rights in the Palestinian territories occupied since 1967. UN doc A /HRC/49/87. .
Klein, N. 2007. The shock doctrine: The rise of disaster capitalism, Macmillan.
LeVine, M. 2016. The Quantum Mechanics of Israeli Totalitarianism. State Crime Journal, 5, 9-31.
Mason, C. 2009. Gaza’s health care system crippled before–and after. CMAJ : Canadian Medical Association journal = journal de l’Association medicale canadienne, 180, 608-609.
Mataria, A., Abu-Hantash, I. & Amer, W. 2008. The “brain drain” of the Palestinian society: with an exploratory study of the health and higher education sectors. Jerusalem and Ramallah: Palestine Economic Policy Research Institute (MAS).
More, A. L. 2006. The Dilemma of aid to the PA after the victory of Hamas. The International Spectator, 41, 87-94.
OCHA. 2020. Two years on: people injured and traumatized during the “Great March of Return” are still struggling. Available: https://www.ochaopt.org/content/two-years-people-injured-and-traumatized-during-great-march-return-are-still-struggling#ftn3.
Office for the Coordination of Humanitarian Affairs in the Occupied Palestinian Territory (OCHA) 2020. Gaza strip: snapshot. United Nations.
Palestine Central Bureau of Statistics (PCBS). 2022. Percentage Distribution of Current Expenditure on Health in Palestine by Financing Schemes, 2000-2020. [Online]. Available: https://www.pcbs.gov.ps/statisticsIndicatorsTables.aspx?lang=en&table_id=1302 [Accessed 25/04/2022].
Palestinian Central Bureau of Statistics (PCBS) and Palestinian Water Authority (PWA) 2021. Joint press release on the occasion of World Water Day.
Peretz, A., Labay, K., Zonis, Z. & Glikman, D. 2014. Disengagement Does Not Apply to Bacteria: A High Carriage Rate of Antibiotic-Resistant Pathogens Among Syrian Civilians Treated in Israeli Hospitals. Clinical Infectious Diseases, 59, 753-754.
Qarmout, T. & Béland, D. 2012. The Politics of International Aid to the Gaza Strip. Journal of Palestine Studies, 41, 32-47.
Roy, S. M. 2016. The Gaza Strip: The Political Economy of De-development, Institute for Palestine Studies USA, Incorporated.
Sahli, Z. T., Bizri, A. R. & Abu-Sittah, G. S. 2016. Microbiology and risk factors associated with war-related wound infections in the Middle East. Epidemiol Infect, 144, 2848-57.
Selbervik, H. B., Norway. Kgl, U., Chr. Michelsens, i. & Norway. Ministry of Foreign, A. 1999. Aid and conditionality : the role of the bilateral donor : a case study of Norwegian-Tanzanian aid relationship, Oslo, Royal Ministry of Foreign Affairs.
Shehada, W., Bouquet, B., Nassar, J., Briody, C., Alfarra, N., Doctor, H. V., Daher, M., Rockenschaub, G., Kirkwood, G., Pollock, A. & Kim, H. J. 2021. Health attacks and protection strategies during Gaza’s Great March of Return: a mixed methods study using data from WHO’s Surveillance System for Attacks on Healthcare. Lancet, 398 Suppl 1, S19.
Shomar, R. 2021. Anti-microbial Resistant Bacteria in Health Care Facilities in Gaza: exploring links with WASH.: Final Report of a pilot study conducted under the GCRF/UK Academy of Medical Sciences Networking Grant.
Smith, R. J. 2015. Healthcare under siege: Geopolitics of medical service provision in the Gaza Strip. Social Science & Medicine, 146, 332-340.
Summerfield, D., Halpin, D., Ang, S., Balduzzi, A., Camandona, F., Tognoni, G., Bono, I., Rui, M. & Agnoletto, V. 2018. The maiming fields of Gaza. BMJ, 362, k3299.
The Lancet 2009. The medical conditions in Gaza. The Lancet, 373, 186.
The World Bank 2021. Economic Monitoring Report to the Ad Hoc Liaison Committee.
Truppa, C. & Abo-Shehada, M. N. 2020. Antimicrobial resistance among GLASS pathogens in conflict and non-conflict affected settings in the Middle East: a systematic review. BMC Infectious Diseases, 20, 936.
Turton, J. F., Kaufmann, M. E., Gill, M. J., Pike, R., Scott, P. T., Fishbain, J., Craft, D., Deye, G., Riddell, S., Lindler, L. E. & Pitt, T. L. 2006. Comparison of Acinetobacter baumannii isolates from the United Kingdom and the United States that were associated with repatriated casualties of the Iraq conflict. J Clin Microbiol, 44, 2630-4.
UN Country Team in the occupied Palestinian territory. 2017. Gaza Ten Years Later [Online]. Available: https://www.un.org/unispal/document/gaza-ten-years-later-un-country-team-in-the-occupied-palestinian-territory-report/ [Accessed].
UN General Assembly 2021. Economic and social repercussions of the Israeli occupation on the living conditions of the Palestinian people in the Occupied Palestinian Territory, including East Jerusalem, and of the Arab population in the occupied Syrian Golan. A/76/94–E/2021/73.
UN Human Rights Council 2018. Report of the Special Rapporteur on the situation of human rights in the Palestinian territories occupied since 1967.
UN Human Rights Council 2019. Human rights situation in the Occupied Palestinian Territory, including East Jerusalem, with a focus on access to water and environmental degradation: Report of the Special Rapporteur on the situation of human rights in the Palestinian territories occupied since 1967. UN report A/HRC/40/73.
UN Human Rights Council 2020. Situation of human rights in the Occupied Palestinian Territory, including East Jerusalem, with a focus on collective punishment; Report of the Special Rapporteur on the situation of human rights in the Palestinian territories occupied since 1967.
UN Human Rights Council 2022. Report of the Special Rapporteur on the situation of Human Rights in the Palestinian territories occupied since 1967. UN doc A /HRC/49/87. .
UN Office for the Coordination of Humanitarian Affairs (OCHA). 2018. Only marginal improvement in humanitarian situation in the Gaza Strip in wake of the intra-Palestinian reconciliation agreement.
UN Office for the Coordination of Humanitarian Affairs (OCHA) 2021. Humanitarian Needs Overview OPT.
UNICEF & WW-GVC 2019. WASH Assessment and Surveillance System in Health facilities in The Gaza Strip. Palestine, Gaza Strip.
United Nations Country Team in the occupied Palestinian territory 2012. Gaza in 2020: A liveable place?
United Nations Relief and Works Agency for Palestine Refugees in the near East. 2022. Where we work: Gaza Strip [Online]. Available: https://www.unrwa.org/where-we-work/gaza-strip [Accessed 28.04.22].
WHO 2014. Gaza strip joint health sector assessment report. Health Cluster in the Occupied Palestinian Territory. Gaza strip, Palestine, 23-25.
WHO 2018. Medical care under siege.: Al Mezan Center for Human Rights,.
WHO 2019. “A One-Year Review of Trauma Data and the Humanitarian Consequences”: Emergency Trauma Response to the Gaza Mass Demonstrations 2018-2019.
WHO 2020. Health conditions in the occupied Palestinian territory, including east Jerusalem, and in the occupied Syrian Golan. A73/15.
World Bank 2016. Public Expenditure Review of the Palestinian Authority: Towards Enhanced Public Finance Management and Improved Fiscal Sustainability. Report No: ACS18454.
World Health Organization 2007. Everybody’s business-strengthening health systems to improve health outcomes: WHO’s framework for action. Geneva.
Zorgani, A. 2013. Injured Libyan combatant patients: both vectors and victims of multiresistance bacteria? Libyan Journal of Medicine, 8, 20325.
[1] Following the democratic election of Islamic Hamas to majority in the Palestinian National Authority in 2006, Israel and key western states responded by boycotting its administration. Diplomatic ties and donor funding were cut, and Israel withheld Palestinian tax revenues, which formed 75% of the budget of the Palestinian National Authority.