COVID-19, global inequalities and colonial legacies: pandemic responses in the UK and Uganda

By Rebekah Merriman*
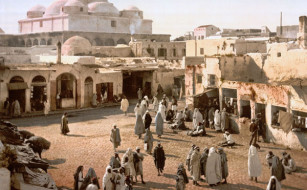
Given the overwhelming speed COVID-19 tore through developed countries, many predicted that developing countries, particularly in Africa, would bear the brunt of the pandemic. For years, the global north-south divide has demonstrated how disparities in wealth and development can dictate health access, experiences and outcomes. Crucially, much of the power, resources and financial successes currently enjoyed by the global north, were gained through the exploitation and impoverishment of the global south, by colonialism and imperialism. As a result, these countries often experience fragile economies and weakened infrastructure. With vast proportions of their populations still living in poverty, they remain at increased risk of poor health and reduced life expectancy.
The difference between the UK and Ugandan health systems exemplifies how the global north-south divide influences countries’ abilities to prepare for and respond to global threats. The UK is one of the world’s richest countries, with a Gross National Income (GNI) per capita of $42,220 and current health expenditure per capita of $4315. Supporting a population of almost 67 million, the National Health Service, is recognised as one of the best health systems in the world. Free at the point of use, it allows access to primary and specialist care with relative ease. Conversely, Uganda is a low-income country, with a GNI per capita of just $680. As a former British colony, government health spending is one hundred times less than the UK, at $43.14 per capita. Supporting over 44 million people, its health system has been fractured over the years by civil wars, disease outbreaks and market-based reforms. Limited public health spending results in an overreliance on private and out-of-pocket payments, further restricting access to healthcare, particularly for the most vulnerable.
As a doctor with several years’ experience in the NHS, I was working in Kampala, Uganda, when coronavirus was first identified as a global threat. It was neither mine, nor many others, prediction that in the months to follow, it would be the UK that was hit hardest by COVID-19, with Uganda remaining relatively unscathed. While at the time of writing the UK has reported almost 4.5 million cases, with over 127,000 deaths, Uganda has had just over 42,000 cases and 346 confirmed deaths. Indeed, the pandemic changed the ‘story of catastrophe’ that has plagued the African continent for years, while also challenging long-standing western supremacy. However, as we move into an era of mass vaccination, global power dynamics are re-emerging to determine which populations get to be protected, and which do not.
Responses to the Pandemic
As the World Health Organization declared a global emergency in January 2020, the UK government was confident it was ‘well-prepared’ for the journey ahead. Indeed, having witnessed the impact of COVID-19 in several other countries, there was time to establish an effective response. However, the months that followed contained significant delays and questionable priorities. Despite adequate infrastructure, intelligence and funding, many lives were compromised by poor policy decisions. For example, in March 2020, the UK government downgraded the threat of covid-19, lowering requirements for personal protective equipment in healthcare settings. It also initially disregarded the widely adopted containment approach of ‘find, test, treat and isolate’, with unrestricted entry into the country and community testing deemed unnecessary. Soon after, with devastating death tolls predicted, the first national lockdown was enforced. People were told to stay at home, while schools and workplaces were closed, and gatherings and travel restricted. Social distancing, handwashing and later, mask-wearing became central to COVID-19 prevention strategy. Since then, the UK has endured varying levels of restriction.
While the UK government has faced significant criticism for its initial response, its economic standing allowed for certain redeeming features. Through releasing emergency funds, it was able to provide some financial protection for people facing unemployment during the pandemic. The furlough scheme received wide praise, ensuring salaries and job security for some through lockdown. Additionally, the UK demonstrated its ability to steer, synthesize and utilise research, being the first country to roll-out the COVID-19 vaccination programme. With 68.2% of its population already having had one vaccine, and 35.9% fully vaccinated, it has remained one of the global leaders in this domain.
Before the first coronavirus case was confirmed in Uganda, the government had already began introducing measures to reduce the likelihood of disease transmission. This involved the closure of schools and businesses, along with the suspension of public gatherings and compulsory quarantine for those arriving into the country. The first case on March 22nd triggered swift and formidable action. By the end of the month, the country was in full lockdown, with a nationwide curfew enforced and both public and private transport suspended. The closure of schools, hospitality and businesses along with the ‘sleep-where-you-work’ policy for market vendors, restricted movement further. The government delivered and disseminated consistent messaging around social distancing, mask-wearing and restricted travel. It also developed a strong capacity to trace and manage cases from early on. Lessons and tactics from recent Ebola experiences were utilised, highlighting the importance of collaboration with communities, civil society and the private sector.
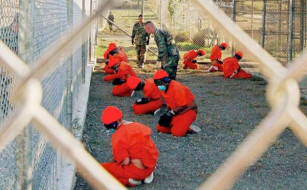
While largely hailed a success, the governments pandemic response has had significant social, political and economic consequences. Aggressive enforcement of COVID-19 laws meant those seen to be flouting guidance experienced harassment, violence and sometimes even death. Along this, came concerns of the marginalisation and targeting of certain groups under the guise of the pandemic, with stories of LGBTQ+ people being ‘outed’ in public prior to arrest and imprisonment. Additionally, President Museveni was accused of utilising the pandemic to push his political agenda and intimidate the opposition during the election period. After several attempts, opposition leader Bobi Wine was arrested for breaking COVID-19 guidelines. This resulted in protests and the killing of dozens of civilians.
Uganda’s limited economic standing has put it at the back of the queue in the global vaccination programme. Currently, it has only received enough doses to fully vaccinate 400,000 people, which represents less than 1% of the population. With an international vaccine shortage, limited personal vaccine purchasing power, and uncertainties around the ability of the COVAX initiative to ensure equitable distribution, the country remains largely unprotected from threats of further outbreaks.
Inequalities Exposed
The initial UK and Ugandan responses significantly influenced their respective rates of COVID-19 cases, hospitalisations and deaths. While on first glance, Uganda appears to have come out victorious, it is important to explore the full impact of virus control measures, as certain consequences remain undetectable within covid-related figures alone.
While both countries went into national lockdown, the reality of these experiences differ drastically. In the UK, for example, housing is generally more secure and spacious, with higher standards of living expected particularly for the upper-and middle-classes. For many, this resulted in quarantining that posed only mild inconvenience and discomfort. Additionally, with fewer transport restrictions, access to basic amenities wasn’t significantly disrupted.
In Uganda, however, especially for the many living in overcrowded city dwellings or multiple occupancy rural households, lockdown brought unique challenges. In the context of aggressive enforcement and transport bans, access to basic foods, treatments and services was significantly limited. This resulted in many preventable health deteriorations and deaths, seen already within maternal and child data. It is argued that strict lockdowns may do more harm than good in global south settings; through the disruption of livelihoods and health care, many more are subject to diseases of poverty and malnutrition.
Inadequate responses in Uganda may have exacerbated this further. For example, tackling food insecurity was highly politicized by the government, firstly by threatening other politicians disseminating food with arrest and murder charges, then later providing food relief only to certain areas of opposition stronghold. Additionally, unlike the UK, Uganda does not have the capacity to provide financial support to those facing unemployment during the pandemic. Instead, many people reliant on daily-wages from the informal sector, were left with little earning capacity and no protection. This results in millions facing worsening impoverishment.
During the pandemic, the internet and digital devices have played key roles in tracking cases, obtaining information, and booking interventions. However, as the world moves online, there is increasing concern that those without access to these resources are left behind. Several papers have explored how this often affects already marginalised communities in Uganda, with women, the disabled and the poor particularly disadvantaged. The digital divide not only exposes inequalities within societies, but also exacerbates the vast inequalities between societies, with devastating health consequences.
In a similar way, the global vaccine divide is determining who has access to vaccines and who doesn’t. Despite Uganda’s best efforts to curb the spread of the virus, global power dynamics influence longer-term complications and consequences. There exists huge disparities in vaccination programmes between the global north and south, putting many already vulnerable populations at increased risk as the world opens up.
The UK and Uganda pandemic responses demonstrate a curtailment of certain human rights and freedoms. It is legally and politically acknowledged that the existence of public health emergencies may justify the necessary and temporary violation of these rights for the protection of health. Alongside this, comes the acceptance that low-income countries may have a lower threshold before such a justification could be relied upon, due to social and economic vulnerabilities.
In Uganda, there are concerns that human rights violations seen within the COVID-19 response were disproportionate and unreasonable. With the world looking inwards, infringements may have been able to continue longer or extend further than the emergency situation required. Indeed, some have criticised the global north for not doing more. However, the UK may have also used the pandemic for political and financial gain, and has encountered growing concerns around limiting individual freedoms through excessive expansion of police power. Additionally, the UK pandemic exposed vast health disparities within vulnerable populations, particularly among poor and racialised communities. Despite key recommendations, the government has done little to mitigate these additional risks.
While human rights concerns may manifest differently depending on the setting, both violating rights and letting rights be violated can result in the loss and limitation of life and so should be criticised accordingly.
The Support Given
The UK has been criticised for looking inwards during the crisis. With ample resources, knowledge and power, it could not only have prevented a large-scale disaster at home but could have also supported its former colonies in their efforts. Comparing the £1.3 million grant to strengthen the Ugandan health response to the billions spent on its own test and trace initiative, underscores the negligible impact of such contributions. Additionally, the UK government has recently decided to cut foreign aid in order to cover the costs of COVID-19 at home. There are growing concerns that this will further limit the global vaccine roll out and widen the increasing north-south divide.
While Uganda didn’t appear to need much external help initially, with the anticipation of an imminent second surge, there is an urgent need to vaccinate its population. Even though Uganda has received donations of 800,000 vaccines, more equitable access and distribution is desperately needed to inoculate the country’s 44 million citizens. Yet, as the cost of the COVID-19 response rises and external support is needed, the already existing significant debts have increased exponentially resulting in calls from President Museveni for the cancellation of African debt, to allow countries to fight the virus on their own terms. This, as opposed to foreign aid, may better ensure local actors can determine where funds should be spent.
Colonial Legacies
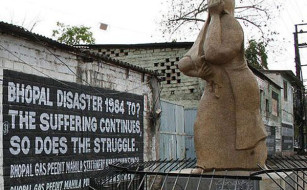
While the initial global COVID-19 outbreak didn’t fit the narrative of Western supremacy and African catastrophe, deeply ingrained power asymmetries between the global north and south are determining which regions will get to live in a post-COVID era. Colonial legacies continue to shape government’s capacity to respond to the complexities of the pandemic and support the health and economic rights of its people.
A year on, longer-term economic crises are set to continue, particularly devastating the global south. Chronic food insecurity, further preventable deaths and restricted access to basic goods and services are all likely. Alongside this, delayed but devastating surges are becoming a reality. With global north aid drying up, the ability of governments to sustain populations living in poverty remains uncertain. Globally co-ordinated responses are crucial, and must include redistributions of wealth, reparations and the democratization of power. Without these, global inequalities are set to deepen.
Rebekah Merriman is a junior doctor currently undertaking a MSc in Global Public Health at Queen Mary University of London.